Introduction: Your Gut—The Unsung Hero of Your Health
Common expressions like having a “gut feeling” or feeling “butterflies in your stomach” are more than just colorful metaphors; they are a reflection of a profound biological reality. These phrases point to a deep, intricate communication network that links our digestive system to our overall state of being. The gut is not merely a passive tube for processing food; it is an intelligent, dynamic system that serves as the foundational pillar of our physical immunity, mental clarity, and emotional balance. Often referred to as the body’s “second brain,” the state of our gut has far-reaching implications for nearly every aspect of our health.
In an age where digestive issues affect millions and confusion about wellness is rampant, understanding the principles of gut health is more critical than ever. This guide is designed to serve as a comprehensive, science-backed roadmap to digestive wellness. It will demystify the complex inner workings of the gastrointestinal system, introduce the trillions of microorganisms that call it home, and explore their staggering influence on the entire body. By journeying from foundational knowledge to a multi-layered action plan, this guide provides the essential tools to recognize signs of imbalance and take decisive steps toward restoring and optimizing gut health for a lifetime of well-being.
Section 1: Gut Health 101: Understanding Your Inner Workings
To embark on the journey toward digestive wellness, it is essential to first understand the fundamental concepts and the intricate machinery at work within the body. This section provides a clear definition of gut health and a guided tour of the digestive system, revealing a process far more complex and elegant than simple food processing.
What is Gut Health? A Clear Definition
Gut health refers to the overall well-being and optimal function of the entire gastrointestinal (GI) system. While there is no single, universally accepted medical definition, the term generally describes a state of having a healthy, balanced gut microbiome and experiencing limited or no adverse digestive symptoms. The primary functions of this system are to digest food, absorb the nutrients necessary for energy, growth, and tissue repair, and effectively eliminate waste products from the body. A healthy gut performs these tasks efficiently and without discomfort, forming the bedrock of systemic health.
Anatomy of the Digestive System: A Guided Tour
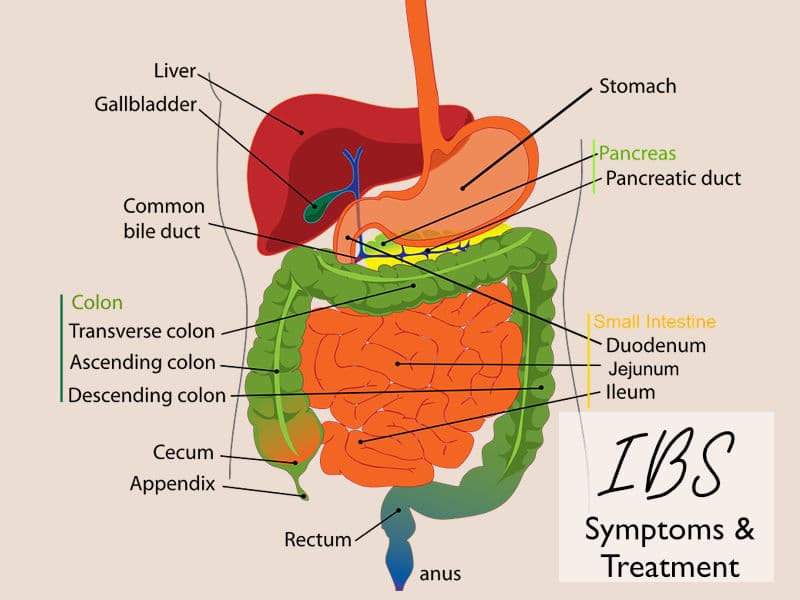
The GI tract is a continuous passageway that extends approximately nine meters (30 feet) from the mouth to the anus, comprising a series of specialized organs working in concert. Understanding the journey food takes through this system illuminates the importance of each component.
- Mouth (Oral Cavity): Digestion begins here, long before food reaches the stomach. The teeth perform mechanical breakdown by chewing, while saliva lubricates the food and initiates chemical digestion. Saliva contains enzymes like salivary amylase, which starts breaking down carbohydrates, and lingual lipase, which begins the digestion of fats (lipids).
- Esophagus: After swallowing, food travels down the esophagus, a muscular tube that uses coordinated, wave-like contractions known as peristalsis to transport its contents to the stomach.
- Stomach: This J-shaped organ acts as a temporary storage container and a powerful digestive chamber. Its muscular walls contract to mix and churn food with potent gastric juices, forming a semi-liquid mixture called chyme. These juices contain hydrochloric acid, which maintains a highly acidic environment with a pH between 1.5 and 2.0. This acidity serves a dual purpose: it activates enzymes like pepsin to break down proteins and, crucially, it acts as a first line of defense, destroying most of the potentially harmful microorganisms ingested with food. The stomach also secretes a substance called intrinsic factor, which is essential for the absorption of vitamin B12 later in the small intestine.
- Small Intestine: This long, coiled tube is where the vast majority—around 90%—of nutrient absorption occurs. It is divided into three segments: the duodenum, jejunum, and ileum. The inner lining of the small intestine is covered with millions of tiny, finger-like projections called villi, which are themselves covered in even smaller projections called microvilli. This structure creates an enormous surface area, maximizing the capacity for absorption. Here, chyme is mixed with digestive enzymes from the pancreas and bile from the liver and gallbladder, which break down fats, proteins, and carbohydrates into absorbable molecules that pass into the bloodstream.
- Large Intestine (Colon): What remains of the food—mostly water, electrolytes, and indigestible fiber—moves into the large intestine. The primary roles of the colon are to absorb the remaining water and electrolytes and to house the vast majority of the gut microbiome. The microbes here perform the final stages of digestion, fermenting fiber and producing beneficial compounds.
- Rectum and Anus: The large intestine compacts the remaining waste material into stool, which is stored in the rectum before being eliminated from the body through the anus.
This intricate process reveals that the digestive system is far more than a simple plumbing network. It is an active and intelligent system of coordinated chemical and mechanical actions. The stomach’s intense acidity, for example, is not just a tool for digestion but a critical protective barrier. Any factor that compromises this acidity, such as the frequent use of acid-blocking medications, can weaken this defense, potentially allowing more pathogens to survive and disrupt the delicate microbial balance further down the digestive tract.
Section 2: Meet Your Microbiome: The Trillions of Tenants Within
Deep within the gastrointestinal tract resides a bustling, microscopic world that is central to the concept of gut health: the gut microbiome. This complex community of microorganisms is not a passive bystander in digestion but an active and essential partner in maintaining our overall well-being.
What is the Gut Microbiome? Your Inner Ecosystem
The gut microbiome is the collective name for the trillions of microorganisms—including bacteria, viruses, fungi, and archaea—that live in the digestive tract, primarily in the large intestine. This community contains up to 1,000 different species of bacteria and is so vast that the number of microbial cells in the body is comparable to the number of human cells.
It is helpful to think of the microbiome as a diverse and vibrant native garden that, when healthy and thriving, provides nourishment and protection. Each person’s “garden” is unique, with its initial seeds planted at birth and its composition continuously shaped by genetics, environment, diet, and lifestyle choices throughout life.
The Importance of Diversity: A Symphony of Species
A key indicator of a healthy gut microbiome is its diversity—the presence of a wide variety of different species. A rich and diverse ecosystem is more resilient and robust. It can perform a wider range of functions and is better equipped to keep potentially harmful microbes in check. When diversity is low, the ecosystem becomes vulnerable, allowing a few opportunistic “weeds” or pathogenic species to overgrow and dominate the environment. This imbalance, known as dysbiosis, can manifest as a loss of beneficial bacteria, an overgrowth of harmful ones, or a general decline in microbial diversity, and it is linked to a host of health issues.
The Microbiome’s Critical Job Roles
These microscopic tenants perform a wide array of functions that are vital for human health. Their roles extend far beyond simple digestion.
- Digestion and Nutrient Extraction: The human body lacks the enzymes needed to break down certain complex carbohydrates, most notably dietary fiber. Gut microbes, however, are equipped with a vast arsenal of enzymes that can ferment these fibers, unlocking otherwise inaccessible nutrients and energy from our food. This partnership means our digestive capacity is far greater than what our own cells can achieve alone. What is often termed “indigestible” fiber is, in fact, the primary food source for this crucial microbial organ.
- Production of Beneficial Compounds: As microbes ferment fiber, they produce a range of beneficial byproducts. The most important of these are short-chain fatty acids (SCFAs), such as butyrate, propionate, and acetate. Butyrate, in particular, serves as the primary fuel source for the cells lining the colon, helping to maintain a strong and healthy gut barrier. SCFAs also have powerful anti-inflammatory properties and play a key role in signaling throughout the body.
- Vitamin Synthesis: The gut microbiome is a veritable vitamin factory, synthesizing several essential nutrients that the body cannot produce on its own. These include a range of B vitamins (such as folate, biotin, and B12) and approximately half of the body’s daily requirement of Vitamin K.
- Protection and Immune Education: A healthy microbiome forms a physical barrier along the intestinal wall, preventing harmful pathogens from taking hold. These beneficial microbes compete with invaders for space and nutrients, effectively crowding them out. Furthermore, the microbiome plays a critical role in educating and regulating the immune system, a process that begins at birth and continues throughout life.
Section 3: The Far-Reaching Influence of Your Gut
The importance of gut health extends far beyond the confines of the digestive tract. Through a series of complex communication networks, the state of the gut and its microbiome influences the immune system, the brain, the skin, and the risk of developing numerous chronic diseases. Understanding these connections reveals why the gut is truly the cornerstone of whole-body wellness.
The Gut-Immune Connection: Your Body’s First Line of Defense
An astonishing 70% of the body’s immune system is located in the gut, making the gastrointestinal tract a primary site for immune activity. This strategic placement allows the immune system to constantly monitor what enters the body and to mount a defense against ingested pathogens. The gut microbiome is an essential partner in this process. From the moment of birth, it begins to “train” the immune system, helping it learn to differentiate between harmless substances like food and beneficial bacteria, and genuine threats like disease-causing microbes.
When the microbiome is in a state of dysbiosis, this educational process can go awry. An imbalanced gut can lead to a dysregulated immune response, contributing to chronic, low-grade inflammation that underlies many health conditions. This can manifest as an increased susceptibility to infections or, in some cases, an immune system that becomes overactive and begins to attack the body’s own tissues, a hallmark of autoimmune diseases.
The Gut-Brain Axis: How Your Gut Governs Your Mood and Mind
The profound connection between the gut and the brain, known as the gut-brain axis, is a bidirectional superhighway of information. This network links the central nervous system (CNS), which includes the brain and spinal cord, with the enteric nervous system (ENS), a complex web of over 100 million nerve cells lining the GI tract that is often called the “second brain”.
Communication flows in both directions through several key channels:
- The Vagus Nerve: This long cranial nerve acts as a direct physical link, sending signals from the gut to the brain and vice versa.
- Neurotransmitters: The gut is a major producer of neurotransmitters, the chemical messengers that regulate mood. In fact, up to 95% of the body’s serotonin, a key mood-stabilizing neurotransmitter, is produced in the gut, along with significant amounts of dopamine. Gut microbes directly influence the production of these chemicals.
- Microbial Metabolites: Compounds produced by the microbiome, such as SCFAs, can enter the bloodstream and travel to the brain, where they can influence its function.
When the gut is inflamed or in a state of dysbiosis, the signals sent to the brain can be disrupted. This can contribute to mental health challenges, including anxiety, depression, and cognitive issues like “brain fog”.
The Gut-Skin Axis: The Secret to a Healthy Glow
The health of the skin is often a direct reflection of the health of the gut. This relationship is known as the gut-skin axis, a bidirectional communication pathway that links intestinal health with skin homeostasis. Gut dysbiosis can compromise the integrity of the intestinal barrier, a condition commonly referred to as “leaky gut.” This allows inflammatory molecules and microbial byproducts to escape the gut and enter the bloodstream. The immune system responds to these circulating substances, triggering systemic inflammation that can manifest on the skin, either causing or exacerbating conditions like acne, eczema, rosacea, and psoriasis.
Gut Health and Chronic Disease: An Emerging Frontier
The interconnectedness of these various “axes” points to a central, unifying mechanism: systemic inflammation originating from an imbalanced gut. Dysbiosis appears to be the root cause, which leads to a compromised gut barrier. This “leakiness” allows bacterial components and other substances to enter the circulation, triggering a body-wide, low-grade inflammatory response. This chronic inflammation is now understood to be a key driver in the development and progression of a wide range of modern chronic diseases.
Emerging research continues to strengthen the links between gut dysbiosis and numerous conditions, including:
- Metabolic Diseases: Obesity, type 2 diabetes, and metabolic syndrome.
- Cardiovascular Disease: The production of certain microbial metabolites like trimethylamine N-oxide (TMAO) has been linked to the hardening of the arteries (atherosclerosis).
- Autoimmune Diseases: Conditions such as inflammatory bowel disease (IBD), which includes Crohn’s disease and ulcerative colitis, as well as rheumatoid arthritis and celiac disease.
- Neurodegenerative Diseases: There is growing evidence suggesting a connection between the gut microbiome and the risk of diseases like Alzheimer’s and Parkinson’s disease.
This body of evidence paints a clear picture: the gut is not an isolated system. Its health, or lack thereof, sends ripples throughout the entire body, influencing everything from daily mood to the long-term risk of chronic illness.
Section 4: Listening to Your Gut: Signs of an Imbalance
The body often sends clear signals when the delicate ecosystem of the gut is out of balance. While some of these signs are obvious and directly related to digestion, many are surprisingly systemic, affecting parts of the body seemingly unrelated to the gut. Learning to recognize both the common and uncommon signs of gut imbalance is the first step toward taking corrective action.
Obvious Red Flags: Common Digestive Symptoms
The most direct indicators of gut distress are those that manifest within the digestive system itself. While experiencing these symptoms occasionally is normal for most people, their persistent or chronic nature can signal an underlying imbalance in the gut microbiome.
Key digestive red flags include:
- Bloating and Excessive Gas: A feeling of fullness, tightness, or visible distension in the abdomen, often accompanied by frequent gas. This can indicate that microbes are improperly fermenting food, producing excess gas.
- Constipation: Infrequent or difficult-to-pass bowel movements. This may be a sign of slow gut motility, which can be influenced by the types of microbes present in the gut.
- Diarrhea: Frequent, loose, or watery stools. This can suggest that the gut is inflamed or that food is moving through the system too quickly for proper water absorption.
- Heartburn/Acid Reflux: A burning sensation in the chest that occurs when stomach acid flows back into the esophagus. This can be a sign of imbalance in the upper GI tract.
- Abdominal Pain and Cramping: General discomfort or sharp, intermittent pains in the abdomen can be a direct result of inflammation or irritation in the gut.
The Surprising Systemic Signals of an Unhealthy Gut
Because of the gut’s extensive influence on the entire body, signs of dysbiosis often appear in seemingly unrelated areas. Recognizing these connections is crucial for identifying the root cause of many chronic complaints.
Less intuitive, systemic signals include:
- Chronic Fatigue and Poor Sleep: An imbalanced gut can disrupt the production of serotonin, a neurotransmitter crucial for regulating sleep cycles. The chronic, low-grade inflammation associated with dysbiosis can also drain energy, leading to persistent fatigue.
- Skin Irritation: As a result of the gut-skin axis, chronic skin conditions like acne, eczema, psoriasis, and rosacea can be signs of internal gut inflammation.
- Mood and Mental Health Issues: The gut-brain axis means that gut inflammation can contribute to anxiety, depression, irritability, brain fog, and difficulty concentrating.
- Autoimmune Conditions: An unhealthy gut can trigger a dysregulated immune response, potentially leading to the development or flare-ups of autoimmune conditions where the body attacks itself, such as Hashimoto’s thyroiditis or rheumatoid arthritis.
- Unintentional Weight Changes: Dysbiosis can impair the body’s ability to absorb nutrients, regulate blood sugar, and store fat, leading to unexplained weight gain or loss without changes to diet or exercise.
- Food Intolerances: The sudden development of sensitivities to foods that were previously well-tolerated can be a sign of a compromised gut lining or an imbalance in the bacteria needed to digest those foods properly.
- Intense Sugar Cravings: An overgrowth of certain types of yeast and bacteria that feed on sugar can drive powerful cravings for sugary and highly processed foods, creating a vicious cycle.
| Common Digestive Signs | Surprising Systemic Signs |
| Bloating and Gas | Chronic Fatigue and Poor Sleep |
| Constipation or Diarrhea | Skin Rashes (Eczema, Acne, Psoriasis) |
| Heartburn and Acid Reflux | Mood Swings (Anxiety, Depression) |
| Abdominal Pain and Cramping | Brain Fog and Difficulty Concentrating |
| Bad Breath | Joint Pain and Inflammation |
| Mucus in Stool | Unexplained Weight Changes |
| Nausea | New Food Sensitivities and Allergies |
Spotlight on “Leaky Gut Syndrome” (Increased Intestinal Permeability)
Many of the systemic symptoms of gut imbalance are linked to a condition known as “leaky gut syndrome.” While not always recognized as a formal medical diagnosis, the underlying mechanism, known as increased intestinal permeability, is a scientifically validated phenomenon.
The lining of the small intestine is a remarkable barrier, designed to be selectively permeable. It is held together by structures called “tight junctions,” which act like gatekeepers, controlling what passes from the gut into the bloodstream. In a healthy gut, only properly digested nutrients, water, and electrolytes are allowed through.
In a state of increased intestinal permeability, factors like poor diet, chronic stress, and dysbiosis can cause these tight junctions to loosen or become damaged. This creates gaps in the intestinal wall, allowing undigested food particles, toxins, and bacterial components to “leak” into the bloodstream where they do not belong. The immune system identifies these substances as foreign invaders and mounts an attack, triggering a widespread inflammatory response. This chronic, systemic inflammation is the mechanism that connects a leaky gut to the diverse range of symptoms listed above, from joint pain and skin rashes to fatigue and brain fog.
Section 5: The Ultimate Action Plan for a Healthier Gut
Restoring and maintaining gut health is an achievable goal that involves a holistic approach, combining mindful dietary choices with supportive lifestyle habits. The single most powerful tool for shaping the gut microbiome is diet, but factors like stress, sleep, and exercise also play indispensable roles. This action plan provides a comprehensive framework for nourishing the gut from the inside out.
Part 1: Nourish Your Microbiome – The Pillars of a Gut-Friendly Diet
What one eats directly feeds the trillions of microbes in the gut, determining which species thrive and which diminish. Adopting a gut-friendly diet is about more than just avoiding “bad” foods; it’s about actively cultivating a diverse and resilient inner ecosystem.
Embrace Fiber: The Superfood for Your Microbes
Dietary fiber is the cornerstone of a healthy gut. It plays a dual role: insoluble fiber adds bulk to stool and promotes regular bowel movements, while soluble fiber dissolves in water to form a gel-like substance that slows digestion and serves as the primary food source for beneficial gut bacteria. When microbes ferment soluble fiber, they produce health-promoting SCFAs that reduce inflammation and lower the risk of numerous diseases. Aiming for a daily intake of 25-38 grams of fiber from a variety of plant sources is recommended.
- Excellent sources of fiber include: legumes (beans, lentils, chickpeas), whole grains (oats, quinoa, barley), fruits (apples, berries, bananas), and vegetables (broccoli, Brussels sprouts, carrots).
Power Up with Prebiotics & Probiotics
- Prebiotics: These are specific types of fiber that act as a “fertilizer” for beneficial gut bacteria, stimulating their growth and activity. Including prebiotic-rich foods is a powerful way to nourish the existing good microbes. Food sources include garlic, onions, leeks, asparagus, bananas, and Jerusalem artichokes.
- Probiotics: These are live, beneficial bacteria found in fermented foods that can help populate the gut with healthy microbes. Consuming a variety of probiotic foods introduces different strains of bacteria, contributing to a more diverse microbiome. Food sources include yogurt with live active cultures, kefir, sauerkraut, kimchi, miso, and kombucha.
Harness the Power of Polyphenols
Polyphenols are natural compounds found in plant-based foods that are packed with antioxidants. They have a potent anti-inflammatory effect and also act as prebiotics, feeding beneficial gut bacteria and inhibiting the growth of harmful ones. A diet rich in colorful plants is a great way to ensure a high intake of polyphenols.
- Polyphenol-rich foods include: berries, grapes, green tea, extra virgin olive oil, dark chocolate (in moderation), nuts, and brightly colored vegetables.
Foods to Limit: The Gut Health Saboteurs
Just as some foods build a healthy gut, others can actively harm it. Limiting the following can significantly reduce inflammation and prevent dysbiosis.
- Ultra-Processed Foods: These products are typically low in fiber and high in additives like emulsifiers, preservatives, and unhealthy fats, all of which can disrupt the microbiome, promote inflammation, and contribute to a leaky gut.
- Excess Sugar and Artificial Sweeteners: A high intake of added sugars, particularly high-fructose corn syrup, feeds pathogenic bacteria and yeast, leading to dysbiosis and inflammation. Many artificial sweeteners have also been shown to negatively alter the gut microbiome and can contribute to glucose intolerance.
- Unhealthy Fats and Fried Foods: Foods high in trans fats and excessive saturated fats can reduce microbial diversity and increase the population of inflammation-promoting bacteria.
- Excessive Alcohol: Alcohol can irritate the gut lining, increase intestinal permeability, and negatively alter the balance of the microbiome.
| Foods to Embrace | Foods to Limit |
|---|---|
| High-Fiber Foods (Legumes, Oats, Vegetables) – Feeds beneficial microbes and promotes regularity. | Ultra-Processed Foods (Packaged Snacks, Fast Food) – Contains additives that harm the microbiome. |
| Prebiotic Foods (Garlic, Onions, Bananas) – Acts as “fertilizer” for good bacteria. | Added Sugars (Soda, Candy, Sugary Cereals) – Feeds pathogenic bacteria and drives inflammation. |
| Probiotic Foods (Yogurt, Kefir, Kimchi) – Introduces live, beneficial bacteria. | Artificial Sweeteners (Found in “Diet” Products) – Can negatively alter microbial balance. |
| Polyphenol-Rich Foods (Berries, Olive Oil, Green Tea) – Reduces inflammation and supports good bacteria. | Fried & High-Fat Foods – Promotes inflammation and reduces microbial diversity. |
| Lean Proteins (Fish, Poultry, Tofu) – Supports tissue repair without overloading digestion. | Processed Meats (Bacon, Deli Meats) – Linked to inflammation and increased cancer risk. |
| Healthy Fats (Avocado, Nuts, Seeds) – Provides anti-inflammatory benefits. | Excessive Alcohol – Irritates the gut lining and disrupts microbial balance. |
Part 2: Lifestyle Adjustments for Lasting Digestive Wellness
A truly healthy gut is supported not only by diet but also by a foundation of healthy lifestyle practices. The factors of stress, sleep, and exercise are not isolated from gut health; they are deeply interconnected, creating powerful feedback loops that can either support or sabotage digestive wellness.
- Manage Stress: Chronic stress has a direct physiological impact on the gut. It triggers the “fight-or-flight” response, releasing hormones like cortisol that can alter gut motility, increase intestinal permeability (leaky gut), and change the composition of the microbiome. Implementing regular stress-management practices can calm this response and protect the gut. Effective techniques include deep breathing exercises (such as the 4-7-8 method), meditation, yoga, and journaling.
- Prioritize Sleep: The relationship between sleep and the gut is bidirectional: poor sleep can disrupt the microbiome, and an imbalanced microbiome can impair sleep quality. Sleep deprivation can reduce beneficial bacteria and increase inflammation. Aiming for 7-9 hours of quality sleep per night is crucial. Practicing good sleep hygiene—such as maintaining a consistent sleep schedule, creating a cool and dark bedroom environment, and avoiding screens before bed—can support both sleep and gut health.
- Optimize Exercise: Regular, moderate physical activity is one of the best ways to support a healthy gut. It enriches microbial diversity, improves the production of beneficial SCFAs, and stimulates gut motility, which helps with regularity. A balanced routine that includes activities like brisk walking, cycling, yoga, and core-strengthening exercises is ideal. It is important to note that while moderate exercise is beneficial, excessively strenuous, long-duration exercise can temporarily increase gut permeability and inflammation, so balance is key.
- Stay Hydrated: Water is essential for every stage of digestion. It helps break down food, allows the body to absorb nutrients, and softens stool to prevent constipation. Staying well-hydrated has also been linked to increased diversity of bacteria in the gut.
- Use Antibiotics Wisely: While often medically necessary to fight bacterial infections, broad-spectrum antibiotics are indiscriminate and can significantly disrupt the microbiome by eliminating beneficial bacteria along with the harmful ones. This can lead to a long-term loss of diversity. Antibiotics should only be taken when prescribed by a healthcare professional. After a course of antibiotics, it is particularly important to focus on restoring the gut through a diet rich in fiber, prebiotics, and fermented foods.
These lifestyle factors are deeply intertwined. For instance, chronic stress can lead to poor sleep and cravings for high-sugar comfort foods, creating a vicious cycle that rapidly degrades gut health. Conversely, adopting a positive change in one area, such as incorporating a daily walk, can initiate a virtuous cycle: exercise reduces stress, which in turn improves sleep quality, making it easier to make healthier food choices. This interconnectedness means that starting with one small, manageable change can create powerful, positive ripple effects across one’s entire well-being.
Section 6: Advanced Support for Your Gut Health Journey
While a foundation of diet and lifestyle changes is paramount for gut health, some individuals may benefit from more targeted and advanced support. The world of supplements can be confusing, but certain evidence-backed options can provide a helpful boost. For those with significantly compromised gut function or nutrient absorption issues, Intravenous (IV) Micronutrient Therapy offers a powerful and direct path to cellular nourishment and repair.
Navigating the World of Gut Health Supplements
The market for gut health supplements is vast, but it is important to approach them with an evidence-based perspective. A food-first approach is always the best starting point, but in certain cases, high-quality supplements can complement a healthy lifestyle.
- Probiotics: Probiotic supplements contain live beneficial microorganisms. Their effectiveness is highly strain-specific, meaning different strains offer different benefits, and not all products are created equal. While strong evidence supports their use for specific conditions like preventing antibiotic-associated diarrhea, the evidence for general wellness is still evolving. Some of the most well-researched probiotic strains include:
- Lactobacillus strains: L. rhamnosus GG has been shown to be effective for various types of diarrhea. L. acidophilus may help with cholesterol management and general digestive health.
- Bifidobacterium strains: B. longum BB536 can support regularity and help with occasional constipation. B. infantis has shown promise for improving symptoms of Irritable Bowel Syndrome (IBS).
- Saccharomyces boulardii: This is a beneficial yeast, not a bacterium, that is particularly effective for preventing and treating various forms of diarrhea and supporting individuals with IBD.
- Other Supportive Supplements:
- L-Glutamine: This amino acid is a primary fuel source for the cells lining the intestines and plays a key role in maintaining and repairing the gut barrier.
- Zinc: An essential mineral that supports immune function and helps strengthen the gut lining.
- Fiber (Psyllium Husk): For those who struggle to get enough fiber from their diet, a supplement like psyllium husk can help promote regularity and feed beneficial gut bacteria.
A Deeper Dive: IV Micronutrient Therapy for Enhanced Gut Repair
For individuals with compromised gut health—such as those with IBD, SIBO, or significant leaky gut—the ability to absorb nutrients from food and oral supplements can be severely limited by inflammation and a damaged intestinal barrier. This can create a cycle of malnutrition and further gut dysfunction.
The IV Advantage: Bypassing the Gut for 100% Bioavailability
IV Micronutrient Therapy offers a powerful solution by delivering essential vitamins, minerals, and amino acids directly into the bloodstream. This method completely bypasses the compromised digestive system, ensuring 100% absorption and immediate availability for the body’s cells to use for repair and energy production. This direct delivery makes it an exceptionally effective tool for rapidly replenishing nutrient deficiencies and providing the building blocks needed for gut healing.
The Nava Health Solution
At Nava Health, this advanced approach has been refined into a specialized Gut Health IV therapy, specifically designed to provide targeted, high-impact support for digestive wellness. This therapy is formulated to soothe and support the gut lining, reduce bloating and discomfort, promote a balanced microbiome, and enhance the body’s ability to absorb nutrients from food in the long term.
The key ingredients in the Nava Health Gut Health IV are carefully selected for their synergistic effects on the digestive system:
- L-Glutamine and Taurine: These amino acids are crucial for repairing and maintaining the integrity of the intestinal lining, making them essential for addressing leaky gut and improving barrier function.
- Vitamins (Vitamin C, B-Complex, B12,): This powerful blend of vitamins works to reduce inflammation, support energy metabolism within gut cells, and aid the function of digestive enzymes.
- Minerals (Magnesium, Potassium): These electrolytes are vital for proper muscle function, including the smooth muscle contractions in the intestines that promote healthy motility and prevent constipation.
- Glutathione: As the body’s master antioxidant, glutathione helps protect gut cells from oxidative stress, supports detoxification processes, and reinforces the integrity of the gut barrier.
This IV therapy is an ideal solution for those experiencing chronic digestive discomfort, symptoms associated with leaky gut, or challenges with nutrient absorption. It is not a standalone cure but a strategic component of a comprehensive wellness plan, designed to accelerate healing and enhance the benefits of dietary and lifestyle modifications.
Ready to take a proactive step towards profound gut repair? Learn more and book your Nava Health Gut Health IV therapy today.
Conclusion: Your Path to Lifelong Wellness Starts in the Gut
The journey through the intricate world of the gut reveals a fundamental truth: the health of our digestive system is inextricably linked to the health of our entire body. The gut is not merely a digestive organ but a complex, intelligent command center that influences our immune defenses, our mental and emotional states, and our long-term resilience against chronic disease. Its cornerstone is a diverse and thriving microbiome—a community of trillions of microorganisms that work in partnership with our bodies to extract nutrients, synthesize vitamins, and maintain a delicate balance.
The pillars of gut wellness are built on a foundation of mindful choices. A diet rich in fiber, prebiotics, probiotics, and polyphenols from whole, plant-based foods provides the essential nourishment for our microbial allies. Simultaneously, a conscious effort to manage stress, prioritize restorative sleep, and engage in regular, moderate exercise creates an environment where a healthy gut can flourish.
Improving gut health is a personal journey, not a one-size-fits-all prescription. It begins with listening to the body’s signals—both the obvious digestive cues and the more subtle systemic whispers of fatigue, skin issues, or mood changes. The path forward involves making small, sustainable changes that can create a virtuous cycle of well-being.
At Nava Health, the philosophy is rooted in an integrative and personalized approach to wellness. This means looking beyond symptoms to address the root causes of imbalance. By combining foundational strategies like clinical nutrition counseling with advanced, targeted therapies such as IV micronutrient therapy, it is possible to create a comprehensive plan that not only restores gut health but also optimizes vitality and promotes longevity. The path to a healthier, more vibrant life truly begins in the gut.